Respiratory System
- Resting and respiratory rates and minute volume are higher.
- In trauma, children become tachypneic due to:
- Injury to airways or lungs.
- Compensatory mechanism to shock.
- Pain, fear, anxiety.
- Tidal volumes are approximately 5-7ml/kg.
- Reliant on diaphragm.
- Poor pulmonary reserve.
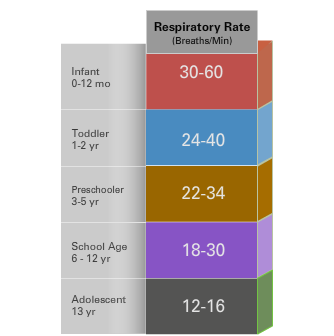
Hypoxia is responsible for the majority of cardiac arrrests in children. The physiologic considerations of the respiratory system in pediatric trauma include: Children have less alveoli and the need to maintain higher respiratory rate to compensate for decreased gas exchange at baseline. Refer to the chart on the right to view the resting respiratory rates in different age groups. In the setting of trauma, children can become tachypneic due to injuries to the airways or lungs, as a compensatory mechanism to hypoperfusion and shock or due to pain, fear and anxiety. As a child becomes hypoxic, work of breathing increases, evidenced by accessory muscle use. Normal tidal volumes are approximately 5-7ml/kg. Excessive volume or pressure during assisted ventilation can result in barotrauma and pneumothorax. The absence of developed intercostal muscles makes young children reliant on the diaphragm to breathe. Restricting diaphragmatic excursion from immobilization or abdominal distension can cause severe respiratory distress. Oxygen consumption and glucose utilization are increased in infants and small children. They also have a decreased functional residual capacity. This may contribute to a rapid onset of hypoxemia in an injured child.